The Society for Maternal-Fetal Medicine (SMFM) 2025 conference at the Gaylord Rockies, January 27–February 1, brought together thought leaders, researchers, and clinicians to discuss the latest advancements in AI, clinical informatics, telemedicine, and maternal health equity. AS Software was proud to be part of the conversation as an exhibitor, where we engaged with industry professionals and gained valuable insights into the future of MFM care delivery.
Here are the key takeaways from the most impactful sessions at this year’s event.
Bringing AI and Informatics into MFM Workflows
The Luncheon Roundtable: Practical Tips for Incorporating AI and Clinical Informatics Into an MFM Practice explored how AI and informatics enhance documentation, clinical decision-making, and workflow efficiency.
Remote Patient Monitoring (RPM):
- NYU‘s 11,000-patient RPM program actively manages 3,000 patients at any time, improving maternal glycemic control and reducing preeclampsia and neonatal hyperglycemia.
- AI-driven predictive modeling is helping providers proactively identify high-risk patients and intervene earlier.
AI in Documentation & Billing:
- AI solutions are streamlining clinical note reconciliation and automating denial letters, saving valuable time for providers.
- NYU has also introduced a HIPAA-compliant ChatGPT platform to assist in clinical decision support and research.
Change Management for AI Adoption:
- Melissa Wong, MD (Cedars-Sinai) highlighted principles from the book “Switch” (Heath & Heath) to drive adoption of AI-driven workflows.
- The key? Find the feeling, shrink the change, and rally the herd—emphasizing incremental improvements, peer learning, and leadership buy-in.
Action Items for Practices:
✔ Pilot AI-generated clinical notes and orders.
✔ Align AI initiatives with institutional goals to drive adoption.
✔ Work with IT to integrate CGM data into the EHR and predict glucose trends.
Addressing Maternal Health Deserts
The Quenching the Gap in Maternal-Fetal Health Deserts session tackled the pressing issue of maternity care facility shortages in rural areas.
The Crisis:
- 35% of U.S. counties lack birthing facilities
- Over 1,100 counties in the U.S. are without a single birthing facility in their country.
- 1 in 12 women in the U.S. are affected by Maternal Health Deserts
- Impacting 7 million women and 500,000 babies.
- 200 rural hospital closures in the past decade have forced patients to travel long distances for maternity care.
- By 2030, the number of obstetricians is expected to decrease by 7% while demand is projected to increase by 4%
Contributing Factors to Maternal Health Deserts
- Geographic isolation
- Economic barriers
- Work Force shortages
- Cultural/language barriers
3 Proposed Solutions:
- Diversifying the Perinatal Workforce: Expanding collaboration between family medicine physicians, midwives, and OB-GYNs.
- Specialized Transport Teams: The Stork 1 team (University of Texas San Antonio) demonstrated how high-performance transport teams reduce risks for high-risk pregnancies in rural areas. States like New Mexico, are awarding an annual rolling $4 million grant for programs like these.
- Telemedicine & Remote Ultrasound: Virtual visits, remote monitoring, and AI-assisted ultrasound are closing care gaps in underserved regions. Practices like Dr. Ruma’s group in New Mexico have used teleultrasound to expand access to care, increasing patient visits from 0 to 5,000 in three years.
Action Items for Practices:
✔ Partner with family medicine and primary care providers to extend maternity care in rural areas.
✔ Create networks that improve continuity and training rural obstetricians.
✔ Develop a telemedicine and RPM blueprint to expand access.
✔ Advocate for policies supporting family medicine’s role in maternity care.
Community Engagement to Improve Perinatal Outcomes
Another key theme at SMFM 2025 was bridging healthcare gaps through community involvement.
Birth Equity Initiatives:
- A July 2021 initiative increased social determinants of health (SDOH) screening from 17% to 100% in hospitals.
- Strategies included standardizing race/ethnicity data and building stronger patient-provider relationships.
Doulas & Community Partnerships:
- Tennessee’s doula training program has improved maternal health literacy, trust, and patient outcomes.
- Hospitals are exploring ways to integrate doulas into clinical teams through targeted training and policy updates.
Action Items for Practices:
✔ Implement SDOH screening in labor & delivery.
✔ Build partnerships with community organizations for better referrals.
✔ Train nurses & staff on doula collaboration.
Obstetric Innovation That Transcends Care Settings
The Philips-sponsored symposium with Perinatal Associates of New Mexico explored how technology is transforming obstetric care across rural and urban settings.
Telemedicine Expansion:
- Ouma, a telehealth company, provides midwifery and behavioral health services to underserved areas, improving maternal health outcomes.
- The growth of remote non-stress tests (NSTs) is making antenatal surveillance more accessible and affordable.
AI-Powered Ultrasound:
- AI applications in ultrasound automation are reducing scan time, increasing accuracy, and improving workflow efficiency.
- Future innovations aim to combine CGM data with ultrasound imaging to predict persistent diagnoses.
Action Items for Practices:
✔ Explore AI-powered solutions to automate ultrasound protocols.
✔ Expand telemedicine services for perinatal care.
✔ Engage with patient communities to understand their digital health needs.
Looking Ahead: How AS Software is Supporting These Advancements
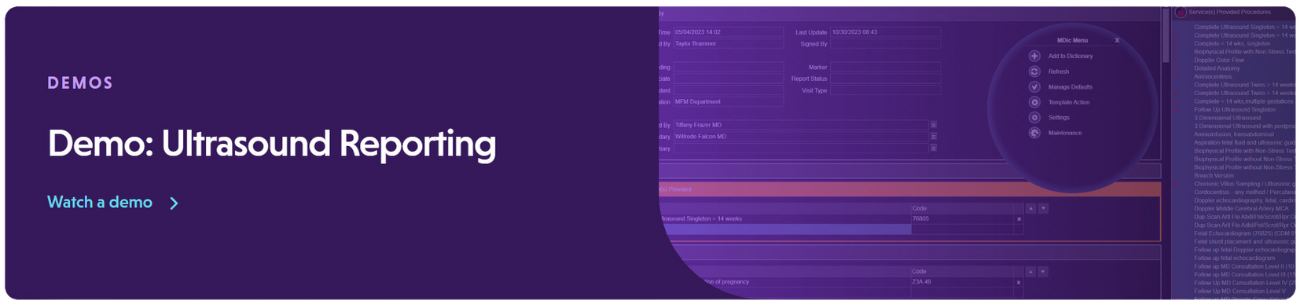
AS Software is committed to supporting MFM providers by delivering cutting-edge ultrasound automation, AI-driven workflow efficiencies, and telemedicine-friendly reporting solutions.
- Remote Diagnostic Access: AS Software enables real-time, cloud-based ultrasound reporting, reducing the need for in-person visits.
- Seamless AI Integration: Our system integrates with EHRs and AI-powered documentation tools, improving efficiency and billing accuracy.
- Scalable Solutions for Rural Care: Our vendor-neutral, cloud-hosted solution supports telemedicine and remote diagnostics, ensuring patients in maternal health deserts get the care they need.
Want to learn more? Connect with our team to discuss how we can help your practice elevate MFM care.
Sources SMFM 2025 Sessions:
Engaging Communities to Improve Perinatal Outcomes
Chair: Ann EB Borders, MD, MPH, MSc (she/her/hers) – Endeavor Health, Evanston Hospital
Chair: Ebony B. Carter, MD (she/her/hers) – University of North Carolina
Chair: Rolanda Lister, MD (she/her/hers) – Vanderbilt University Medical Center
Practical Tips For Incorporating AI and Clinical Informatics Into An MFM Practice
Roundtable Leader: Hye J. Heo, MD (she/her/hers) – NYU Langone Health System
Roundtable Presenter: Melissa S. Wong, MD, MS (she/her/hers) – Cedars-Sinai Medical Center
Obstetric Innovation that transcends care settings
Industry Session Presenter: Michael Ruma, MD, MPH – Perinatal Associates of New Mexico
Industry Session Presenter: Sina Haeri, MD, MHSA – Ouma Health
Industry Session Presenter: Richie Broth, MD – TLC PERINATAL
Quenching the Gap in Maternal Health Deserts
Roundtable Leader: Alixandria F. Pfeiffer, DO – University of Texas Health Science Center at San Antonio